65 year old female with cough-4 months and fever-10 days
Rachana Gangula
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CHIEF COMPLAINTS:
A 65 year old presented with cough since 4 months and fever since 10 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 months back then developed cough associated with sputum , which is whitish in colour, thick, moderate amount, more during nights.
H/o fever since 10 days, high grade a/w chills and rigor , internittent, no evening rise of temperature.
No h/o cold, SOB, chest pain, palpitations, excessive sweating, burning micturition, pedal edema, decreased urine output
H/o increased exposure to dust
PAST HISTORY
Similar complaints in the past 20 years ago , and a/w itching of eyes and relieved with inj.Dexamethasone
K/c/o TYPE 2 DM since 10 years ( gulcoryl- m1 1/2 tab in the morning and half in the night )
N/k/c/o htn, tb, asthma, thyroid disorder, epilepsy
Personal history:-
Patient is moderately built and moderately nourished
Diet: mixed
Appetite: normal
sleep: disturbed since last 10 days
Bowel and Bladder : regular bowel movements, incresed frequency of urination during nights (5/night)
Addictions :- alcohol once in a month but stopped 1 year ago.
Tobbaco (chutta) since last 35 years daily one chutta
General Physical Examination:-
Patient is conscious, coherent and cooperative and well oriented to time, place and person.
Pallor+
Icterus,cyanosis, clubbing, lymphadenopathy and edema are absent.
vitals:-
Temp:- 97.2 ⁰F
BP:- 120/80 mmhg
RR:- 20 cpm
PR :- 78bpm
Grbs :- 173 mg%
Systemic Examination
Respiratory system:
BAE+ NVBS heard
Wheeze in the right supra scapular area.
CVS- s1s2+ no murmurs
Per Abdomen:
Shape is scaphoid
Abdomen is soft and non tender with no organomegaly
Bowel sounds are heard
A vertical surgical scar present from below umbilicus to the pubis symphisis
? Laparotomy i/v/o abdominal mass
CNS- NAD
PROVISIONAL DIAGNOSIS
LRTI ?PNEUMONIA .
Investigations:
ECG
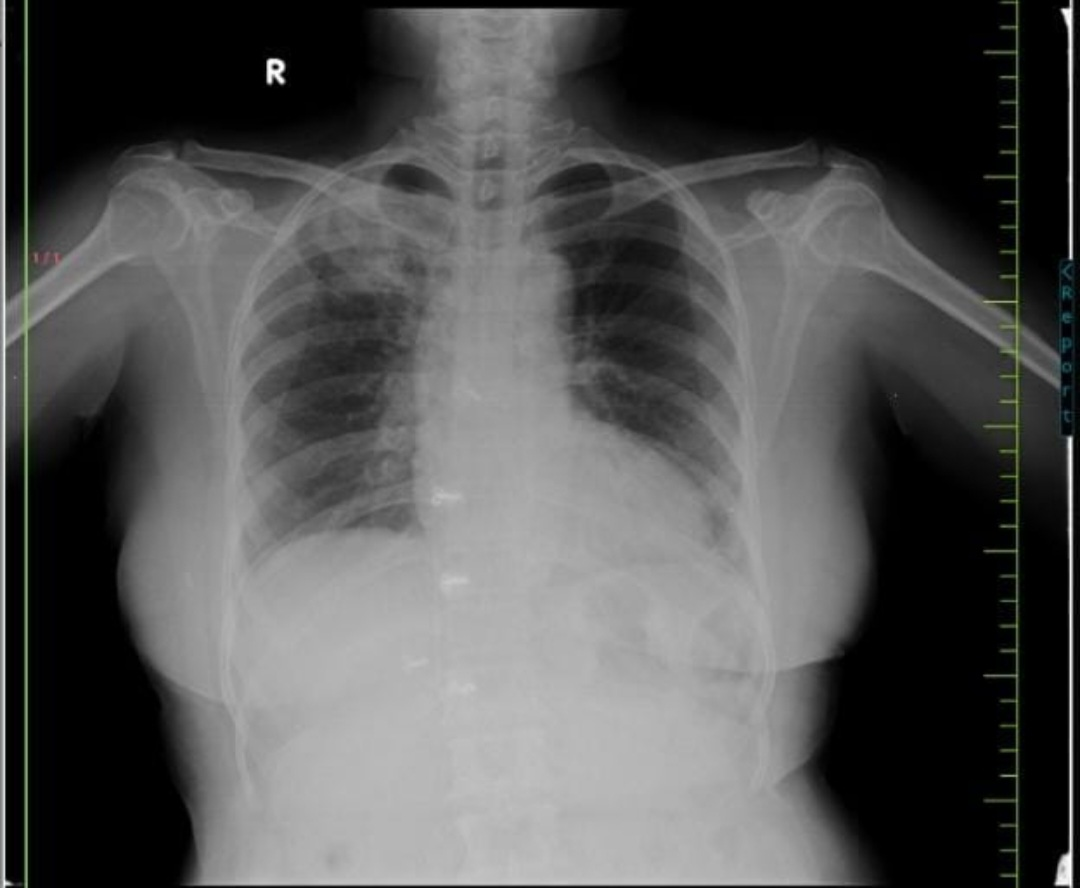
CHEST X RAY
HEMOGRAM:-
HB:- 10
TLC:- 11500
PCV:- 31.9
RBC:- 3.9
PLATELETS:- 3.5
CUE:- normal
PLBS:- 158 mg%
Blood urea:- 39 mg/dl
Serum creatinine:- 0.9 mg/dl
Serum electrolytes:-
Na+ : 139 mEq/L
K+ : 4 mEq/L
Cl- : 102 mEq/L
DIAGNOSIS
? Community Acquired Pneumonia
? Pulmonary TB with rt upper lobe consolidation
K/c/o type 2 DM since 5 years.
TREATMENT
1) Inj. AUGMENTIN 1.2 gm IV/BD for 5 days
2) Tab. AZITHROMYCIN PO/OD for 5 days
3) Tab. METFORMIN 500 mg + GLIMEPIRIDE 1mg PO/BD 1/2 tab




Comments
Post a Comment